Sleep apnea is a sleep disorder that affects millions of people worldwide. This condition is characterized by breathing that repeatedly stops and starts during sleep, causing pauses in breathing, called apneas, that can last from a few seconds to a minute or more. These pauses in breathing can lead to decreased oxygen levels in the body and a variety of health problems.
There are three main types of sleep apnea:
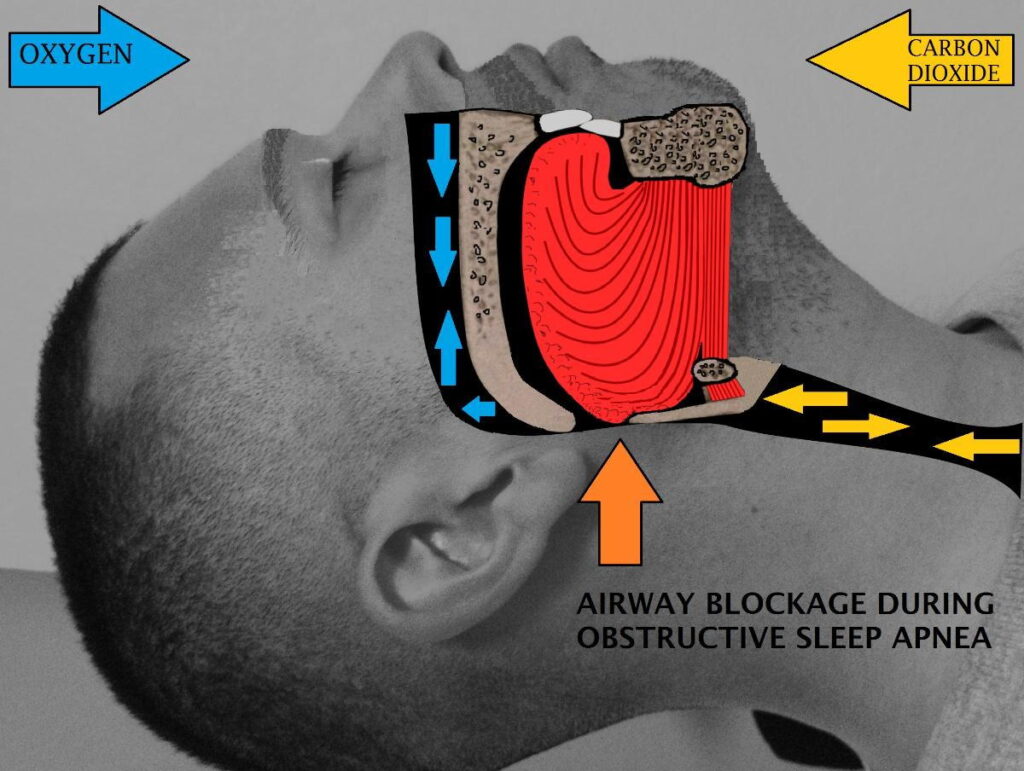
- Obstructive sleep apnea (OSA): This is the most common type of sleep apnea and occurs when the airway is partially or completely blocked during sleep, usually by the collapse of soft tissue in the back of the throat.
- Central sleep apnea (CSA): This type of sleep apnea occurs when the brain fails to send the proper signals to the muscles that control breathing.
- Complex sleep apnea syndrome (also known as treatment-emergent central sleep apnea): This type of sleep apnea is a combination of both OSA and CSA and typically develops in individuals who have been treated with continuous positive airway pressure (CPAP) therapy for OSA.
In this blog post, we will focus on OSA, its causes, symptoms, and treatment options.
What is Obstructive Sleep Apnea (OSA)?
Obstructive Sleep Apnea (OSA) is the most common type of sleep disorder in which a person’s breathing is repeatedly interrupted during sleep. This happens when the muscles in the back of the throat fail to keep the airway open due to the relaxation of the throat muscles, which causes the airway to collapse and become blocked, resulting in a decrease in the amount of oxygen that reaches the lungs. As a result, the brain is signaled to wake up momentarily to restart breathing, which causes a disruption in sleep patterns. OSA can lead to serious health problems and even death if left untreated.
OSA is very dangerous because it can lead to multiple health problems such as hypertension, heart disease, stroke, type 2 diabetes, depression, daytime fatigue and dizziness, and decreased quality of life.
Causes of Obstructive Sleep Apnea (OSA)
There are several risk factors that increase the likelihood of developing OSA, including:
- Age: OSA is more common in people over 40 years of age, as the muscles and tissues that support the airway become weaker with age.
- Gender: Men are more likely to develop OSA than women.
- Obesity: Excess body weight can cause fat deposits to accumulate around the airway, leading to airway obstruction.
- Family history: OSA may run in families due to inherited traits that affect the structure and function of the airway.
- Smoking: Smoking can cause inflammation and damage to the airway, increasing the risk of OSA.
- Alcohol consumption: Alcohol relaxes the muscles in the airway, leading to obstruction and snoring.
- Sedative medications: Certain medications that relax the muscles can worsen OSA symptoms.
- Sleeping on one’s back: can cause the tongue and soft tissues in the throat to collapse, leading to airway obstruction and OSA.
- Nasal congestion and sinus infection: Chronic nasal congestion or inflammation can obstruct the airway and contribute to OSA.
- Enlarged tonsils or adenoids: In children, enlarged tonsils or adenoids can block the airway and cause OSA.
- Medical conditions: OSA may be associated with medical conditions such as high blood pressure, diabetes, and heart disease.
- Hormonal imbalances: Hormonal changes due to conditions such as hypothyroidism or menopause can affect the airway and contribute to OSA.
- Jaw structure: Abnormal jaw structure or a small chin can cause the tongue to fall back into the throat and obstruct the airway during sleep.
- Craniofacial abnormalities: Structural issues in the head and face, such as a deviated septum, a receding chin, or enlarged tonsils or adenoids, can obstruct the airway and lead to OSA
- Certain medications and substances: Some medicines, such as sedatives and muscle relaxants, can cause the muscles in the throat to relax and increase the likelihood of airway collapse during sleep. Alcohol and other depressant drugs can have a similar effect.
Identifying the underlying cause of OSA is essential for developing an effective treatment plan. Seeking medical advice and diagnosis is crucial for managing OSA and reducing the risk of complications.
Sleeping Position and Obstructive Sleep Apnea (OSA)
Sleeping position can also be a cause of OSA. Sleeping on one’s back can cause the tongue and soft tissues in the throat to collapse, leading to airway obstruction and OSA. This is because the force of gravity pulls the tongue and other structures toward the back of the throat, making it more difficult to breathe. Sleeping on one’s side can help alleviate this issue and reduce the risk of OSA.
Signs and Symptoms of Obstructive Sleep Apnea (OSA)
The most common symptoms of OSA include:
- Loud snoring: Snoring is a common symptom of OSA, and it can be loud and disruptive.
- Pauses in breathing during sleep: These pauses in breathing can occur multiple times during the night and can last for several seconds to a minute.
- Gasping or choking during sleep: These symptoms can occur after a pause in breathing and may cause the person to wake up briefly.
- Excessive daytime sleepiness: People with OSA may feel very tired during the day, even after a whole night’s sleep.
- Morning headaches: Headaches can be a symptom of OSA, as the drop in oxygen levels during sleep can cause blood vessels in the brain to widen and result in headaches.
- Difficulty concentrating: Sleep apnea can affect cognitive function and make it difficult to concentrate or focus during the day.
- Memory loss: OSA can lead to a reduction in the oxygen supply to the brain, which can have adverse effects on cognitive function, including memory. OSA affects memory consolidation, which is the process by which new memories are transferred from short-term to long-term storage. OSA has been shown to impact several different types of memory, including verbal memory, spatial memory, and episodic memory.
- Mood changes: Irritability, depression, and anxiety can be symptoms of OSA.
- Dry mouth or sore throat: Breathing through the mouth during sleep can cause a dry mouth or sore throat.
- High blood pressure: OSA can contribute to high blood pressure and other cardiovascular problems
- Decreased libido: OSA can lead to chronic fatigue and daytime sleepiness, which can reduce overall energy levels and decrease interest in sexual activity. Additionally, OSA can lead to decreased oxygen levels in the body, which can affect blood flow to the genital area and decrease arousal and sexual sensation. The stress and anxiety associated with OSA can also contribute to decreased libido, as well as the use of certain medications to treat OSA.
Diagnosing Obstructive Sleep Apnea (OSA)
If you suspect you have OSA, you should consult with your healthcare provider. They may refer you to a sleep specialist who will perform a sleep study to diagnose the condition. During a sleep study, your breathing, heart rate, and other vital signs will be monitored while you sleep.
Treatment Options for Obstructive Sleep Apnea (OSA)
- Lifestyle Changes: Making lifestyle changes, such as losing weight, quitting smoking, avoiding alcohol and sedatives, and sleeping on your side, can help reduce the symptoms of OSA.
- Continuous Positive Airway Pressure (CPAP): CPAP is a standard treatment for OSA. A CPAP machine delivers a continuous flow of air into the airway to keep it open during sleep.
- Oral Appliances: Oral appliances are devices that are worn in the mouth to reposition the jaw and tongue to keep the airway open during sleep.
- Surgery: In severe cases of OSA, surgery may be recommended to remove excess tissue from the throat or to reposition the jaw.
- Positional Therapy: Sleeping in a specific position, such as on your side, can help keep the airway open and reduce the symptoms of OSA.
- Nasal Decongestants: Nasal decongestants can help reduce congestion in the airway, making it easier to breathe during sleep.
- Acupuncture: Acupuncture has been found to be effective in reducing OSA symptoms, such as snoring and daytime sleepiness.
- Weight Loss Surgery: In severe cases of OSA, weight loss surgery may be recommended to reduce the amount of excess fat tissue around the neck.
- Hypoglossal Nerve Stimulation: This treatment involves the use of an implantable device that stimulates the hypoglossal nerve to prevent the airway from collapsing during sleep.
- Inspiratory muscle training (IMT): is a type of exercise designed to strengthen the muscles involved in breathing. It is used as a treatment for respiratory conditions such as chronic obstructive pulmonary disease (COPD), asthma, and neuromuscular diseases.
Inspiratory muscle training (IMT)
Here are some examples of IMT exercises and how to do them:
- Diaphragmatic breathing: This exercise involves deep breathing that emphasizes the use of the diaphragm muscle, which is the primary muscle used for breathing. To do this exercise, sit or lie down in a comfortable position with one hand on your chest and the other on your abdomen. Breathe deeply through your nose, focusing on expanding your abdomen rather than your chest. Exhale slowly through your mouth, letting your abdomen fall inward. Repeat for several minutes.
- Pursed-lip breathing: This exercise can help improve breathing efficiency by slowing down the rate of breathing and promoting deep breathing. To do this exercise, sit or stand in a comfortable position and inhale deeply through your nose. Exhale slowly through pursed lips as if you are whistling. Exhale for two to three times as long as you inhale. Repeat for several minutes.
- Resistive breathing: This exercise involves breathing against resistance, which can help strengthen the respiratory muscles. To do this exercise, use a device such as a spirometer or a respiratory muscle trainer. Breathe in through the device, which will provide resistance to your inhalation. Exhale normally. Repeat for several minutes.
- Inspiratory muscle strength training: This exercise involves using a device that provides resistance to inhalation, such as a handheld device or a machine. The device is set to a specific resistance level, and the person must inhale against the resistance for a set number of breaths or for a particular length of time. Over time, the resistance can be increased to continue to challenge the inspiratory muscles.
- Segmental breathing: This exercise is similar to diaphragmatic breathing but focuses on expanding specific areas of the lungs. To do this exercise, place your hands on different areas of your ribcage (e.g., upper chest, middle chest, lower chest). Breathe in deeply, focusing on expanding each area of your ribcage one at a time. Exhale slowly. Repeat for several minutes.
- Flow-oriented incentive spirometry: This exercise involves using a device called an incentive spirometer, which helps to improve lung function by promoting deep breathing and airway clearance. To do this exercise, sit up straight and place the mouthpiece of the spirometer in your mouth. Take a deep breath in through the mouthpiece and hold it for as long as you can. Exhale slowly and repeat for several breaths.
- Paced breathing: This exercise involves slowing down the rate of breathing and focusing on breathing rhythm. To do this exercise, breathe in for a count of four, hold your breath for a count of four, and then exhale for a count of four. Repeat for several minutes.
- High-intensity interval training (HIIT): for the inspiratory muscles: This exercise involves using a machine or device that provides high levels of resistance to inhalation. The person must inhale against the resistance for a short period of time (e.g., 30 seconds), followed by a rest period. This cycle is repeated several times, with the goal of improving inspiratory muscle strength and endurance.
It is essential to consult with a healthcare professional before starting any new exercise program, including IMT. They can help you determine which exercises are appropriate for your specific condition and provide guidance on how to do them correctly.
Chiropractic care for Obstructive Sleep Apnea (OSA)
Chiropractic care is a non-invasive approach to treating a variety of health conditions, including obstructive sleep apnea (OSA). While many people may not initially consider chiropractic care as a treatment option for OSA, there is growing evidence to suggest that certain chiropractic techniques can be effective in improving sleep quality and reducing the symptoms of OSA.
Chiropractic care focuses on correcting dysfunctions in the spine and other joints in the body. These can interfere with the proper functioning of the body and the nervous system, leading to a range of health problems. By correcting dysfunctions, chiropractors aim to improve body function and promote overall health and wellness.
When it comes to OSA, chiropractic care can be beneficial in several ways. Here are some specific ways that chiropractic care can help with OSA:
- Correcting spinal dysfunctions: Lack of proper motion, immobile joints, and bad posture in the cervical spine (the neck) can contribute to OSA by putting pressure on structures that control the muscles involved in breathing. Chiropractic adjustments can help correct these problems and alleviate this pressure, improving nerve function and reducing the risk of OSA.
- Reducing muscle tension: Tension in the muscles of the neck and jaw can also contribute to OSA by narrowing the airway and making it more difficult to breathe. Chiropractic techniques such as soft tissue massage and trigger point therapy can help reduce muscle tension, making it easier to breathe during sleep.
- Improving overall posture: Poor posture can contribute to a range of health problems, including OSA. Chiropractors can help patients improve their posture through exercises and adjustments that target the spine and other joints. By improving overall posture, patients may be able to reduce the risk of OSA and enhance their quality of sleep.
- Addressing other underlying health issues: OSA is often associated with other health problems, such as high blood pressure, stress, poor sleep hygiene, and obesity. Chiropractors can work with patients to address these underlying issues, helping to reduce the severity of OSA and improve overall health and wellness.
- Developing long-term treatment plan for home, including therapeutic exercises, Inspiratory muscle training (IMT), and lifestyle modifications.
- Craniofacial bones mobilization and adjustment: There is some evidence to suggest that chiropractic adjustments can have a positive impact on craniofacial abnormalities and immobility that can contribute to obstructive sleep apnea (OSA). Chiropractic adjustments or manual manipulations of the joints aim to improve joint mobility and positioning, reduce pain, and enhance functions. Craniofacial abnormalities such as a deviated septum, a receding chin, or enlarged tonsils or adenoids can obstruct the airway and lead to OSA. Chiropractic adjustments may be able to address some of these issues by improving mobility and positioning of the joints.
It is important to note that chiropractic care is not a substitute for other treatments for OSA, such as continuous positive airway pressure (CPAP) therapy. However, it can be a helpful adjunct therapy that may help improve sleep quality and reduce symptoms.
Conclusion
In conclusion, OSA is a serious sleep disorder that can have significant health consequences if left untreated. Fortunately, there are effective treatment options available. If you or someone you know is experiencing signs and symptoms of OSA, it is vital to seek medical attention. Remember, a good night’s sleep is essential for optimal health and well-being.
#sleepapnea #snoring #OSA #healthysleep #sleepdisorder #CPAPtherapy #inspiratorymuscletraining #obesity #quit smoking #chiropractic #chiropractor #familyhistory #sleepapneatreatment.
